Highlights
- All patients presenting to the office as transgender need to have a thorough history taken that includes: history of gender identity, past medical history that focuses on conditions that may affect future cross-sex hormones, social history focusing on social supports and past discrimination/abuse, medication history that focuses on current/past use of hormones (both prescribed and illicit), mental health history, substance abuse history, and a detailed sexual health history.
- A physical exam should be performed on all patients including a genital exam to rule out a possible intersex condition (if this has not been done by a previous physician). Patients may be sensitive to certain parts of the physical exam and patient’s boundaries should always be respected.
- Consider referral to a mental health professional for all patients.
Overview
Adults who identify as transgender may present to your office in many different capacities. You may have a patient who is disclosing their transgender identity for the first time and is unsure of what to do. You may have a patient who has done extensive research on their own and appears quick well-versed in the various medical and surgical options and very sure about their needs. You may have a patient who is already on a stable dose of cross-sex hormones and simply needs the occasional check-in. Alternatively, you may have a patient who has been self-treating with cross-sex hormones purchased from the internet and has not yet had a proper evaluation by a health care professional.
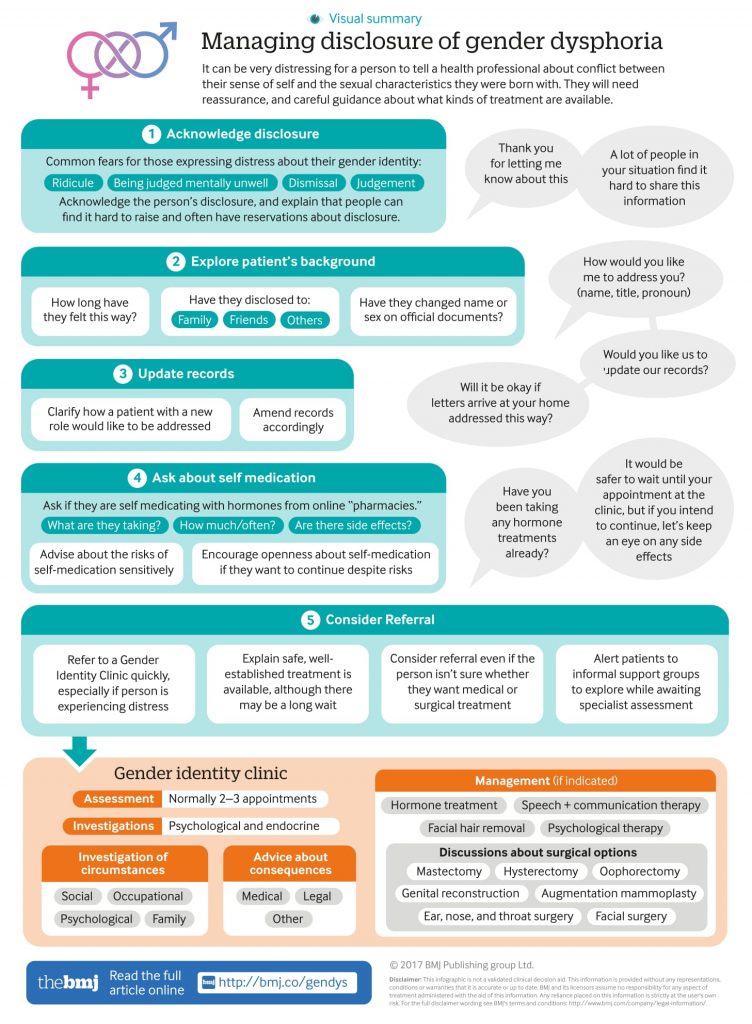
Regardless of how the patient presents, take comfort in the fact that managing this patient is not a quick ten minute appointment, even for the most experienced of healthcare professionals. The initial management of a patient presenting as transgender is best done over several appointments, and often in conjunction with other healthcare professionals, especially a mental health professional (MHP). The graphic below is an example of how one might approach these encounters.
History Taking
There is likely too much information to cover during the initial visit or you may feel some of the more personal questions would be better left for a later appointment, but eventually all of the following should be covered.
History of Gender Presentation
First, acknowledge that this is often a difficult topic to bring up and that you are ready to support them. See Office Tips for suggestions on making your office more LGBTQ friendly. Begin with open ended questions to allow the patient to guide the initial conversation. See some sample questions from the Gender-affirming Care for Trans, Two-Spirit, and Gender Diverse Patients in BC: A Primary Care Toolkit for some more direction.
You can also refer to the official diagnostic criteria for gender dysphoria in the DSM 5 for some guidance as to the types of distress you may wish to enquire about. Determine how long they have identified as transgender and explore their childhood/adolescence experience including puberty (remember, not all adult trans patients identified as transgender as a child). Determine whether or not the have sought medical management or support in the past (if so, attaining these past records can be very helpful). An effort should be made to assess the impact of their trans identity on employment, housing, family, relationships, and economic wellbeing. You make gather a lot of your social history during this part of the conversation as you get a sense of the patients experience and support system.
It is also important to ask how they now wish to be addressed – what pronouns they prefer and whether they have a new or preferred name. It is important to suss out the nuances of this in terms of whether or not they would like their clinic file officially changed, whether they want office staff aware so they can address them appropriately, and whether or not messages can be left at home using the preferred name.
Past Medical History
You may already have a good sense of the patient’s past history, but it is important to review certain risk factors and diagnoses that may preclude a patient from potential cross-sex hormone treatment. It is also important to take some time to review preventative medicine and ensure they are up to date with vaccinations and screening tests (pap smears, mammograms, STI screening, etc.).
It is important to inquire about the following in each group of patients:
- FtM: Heart disease, hypertension, diabetes, hyperlipidemia, hepatic dysfunction, polycythemia, venous thromboembolism or hypercoagulable state, obesity, chronic respiratory disease, sleep apnea, (androgen-sensitive) epilepsy, migraines, oligo/amenorrhea, psychiatric disorders, substance use/abuse, polycystic ovarian syndrome, estrogen-sensitive neoplasms;
- MtF: Heart disease, cerebrovascular disease, hypertension, diabetes, hyperlipidemia, hepatic dysfunction, venous thromboembolism or hypercoagulable state, obesity, begin intracranial hypertension, psychiatric disorders, substance use/abuse, personal or family history of breast cancer, personal or family history of porphyria.
Surgical History
Given the higher proportion of transgender individuals that have co-morbid mental health diagnoses, it is very important the screen for signs of any major mental illnesses. This includes screening for depression/suicidality, symptoms of mania/hypomania, psychosis, and eating disorders. It is also important to rule out any psychiatric conditions that could be mimicking gender dysphoria such as psychotic or dissociative disorders or body dysmorphic disorder. You must also inquire about what, if any, treatment they have had for any mental health diagnoses (counselling, medication, etc.). Have they seen a MHP in the past or currently that has addressed their gender identity?
Family History
Take note of any clotting disorders, cardiovascular disease, hypertension, diabetes, mental illness, or cancer (specifically breast, ovarian, uterine, or prostate).
Medications
This includes current prescribed medications and supplements as well as any current or past use of hormones, either obtained through another physician or through illicit means, like the internet. It is especially important to determine a detailed hormone history if the hormone administration had not been previously supervised by a physician (timeline, doses, route, adverse reactions, etc.).
Social History
It is crucial to understand who their support system includes and who is aware of their gender identity. Who do they live with and do they feel comfortable there? Do they have secure housing? Is their family aware? If so, are they supportive? If unaware, why, and does the patient hope to disclose this to their family in the future? Do they have a current partner? Are they aware and supportive? Are there any friends that have been there for the patient? Also determine whether they are in school or working and whether they have faced any discrimination related to their gender identity. Have they been bullied, harassed, or abused? Do they have financial concerns? Are they smoking, drinking alcohol, or doing other illicit substances? Do they abuse any prescription drugs? Do they have a history of IV drug use or sharing hormone needles; have they been recently screened for HIV or hepatitis? It is also important to get a sense of the patient’s overall healthy lifestyle in terms of diet, exercise, and adequate sleep.
Sexual History
A detailed sexual history is important to ensure proper STI screening and education of safe sexual practices. Does the patient have a current partner; are they male, female or transgender? Are they aware and supportive of the patient’s gender identity? What is the patient’s sexual orientation? What specific sexual acts have they participated in (oral, vaginal, anal intercourse); do they avoid certain sexual encounters because of their gender dysphoria (e.g., a transwoman who is uncomfortable using her penis for penetrative sex)? How many sexual partners have they had ever/in the past 6 months; have they ever take money or drugs for sex? Have they ever been sexually assaulted? Do they have a history of STIs, were they appropriately treated? When were they last screened for STIs? Are they using adequate and consist protection from STIs and pregnancy? Have they even been pregnant? Included in the sexual history should be a conversation about libido, as both male and female hormone therapy can affect this.
Physical Exam
Blood pressure (goal < 140/90), height, weight, abdominal circumference.
Used to rule out any major medical co-morbidity and as an opportunity to offer appropriate disease screening. Build rapport by explaining each part of the exam to the patient and defer any parts of the exam that the patient is uncomfortable with. Sensitive exams can be managed in a variety of ways, depending on patient preference. Some patients prefer the exam to be done as quickly as possible, while others require a slow pace or even light sedation. It is important to rule out a possible intersex condition as an alternative explanation for gender dysphoria and this requires a genital exam. It is important that the patient understands why this exam is being performed and that they have given consent. Often this exam will be delayed until a later appointment after rapport as been established. The chest may also warrant examination depending on the situation (e.g., in MtF patients who would like their future breast development tracked by the physician).
It is worthwhile, to ask the client about preferred words for any body parts (ex- “chest” instead of “breasts” in a FtM patient).
The following are possible physical exam findings as per Transgender Primary Medical Care: Suggested Guidelines for Clinicians in British Columbia:
FtM patients may have beard growth, clitoromegaly, acne, and androgenic alopecia. Those who have bound their breasts for years may have a rash or yeast infection of the skin under the breasts. Post-operative FtM patients after chest surgery will have scar tissue consistent with the type of procedure, and may have large nipples or small grafted nipples (depending on the technique used). The FtM neophallus created from the release of an augmented clitoris looks like a very small penis; a grafted penis constructed by phalloplasty will be adult-sized but more flaccid than in the natal male (erection is obtained through use of a stiffener or pump).
MtF patients may have a feminine breast shape and size, often with relatively underdeveloped nipples; breasts may appear fibrocystic if there have been silicone injections. Galactorrhea is sometimes seen in MtF patients with high prolactin levels, especially among those using breast pumps to stimulate development. There may be minimal body hair, with variable facial hair (depending on the length of time on hormones and manual hair removal treatments such as electrolysis). Testicles may become small and soft; defects or hernias at the external inguinal ring may be present due to the practice of “tucking” the testicles up near (or into) the inguinal canal. Post-operative MtF patients may have undergone breast augmentation with implants. MtF genital surgery typically involves simultaneous removal of the penis/testicles and creation of a neovagina. Some patients may just have the testes removed, prior to or instead of vaginoplasty. There may be varying degrees of labial reconstruction and clitoral hooding, depending on the completion of surgical revisions. The neovagina typically appears less moist than in natal women, and may be stenosed internally if the patient does not dilate daily or is not sexually active.
Assessment and Plan
Develop a plan with the patient for the next few appointments. There is no specific timeline or number of appointments to which a patient must adhere, but usually patients are seen multiple times over a 2-3 month period (especially if the patient is new to you) in order to assess and optimize readiness for hormone therapy if this is in keeping with patient goals.
- Mental Health: Historically, all patients were referred to a MHP for a formal diagnosis of gender dysphoria. While the current WPATH standards of care still place a strong emphasis on specialist referrals for psychological assessment prior to medical or surgical treatment, the paradigm is beginning to shift. As management evolves there is beginning to be a shift from the standards of care model towards an informed consent model which many clinics have adopted. This model de-emphasizes the need for external evaluations by mental health professionals or the diagnosis of “gender dysphoria”, and focuses on the patient’s capacity and right to choose appropriate management with guidance from their prescribing physician. This shift is allowing primary care providers to undertake their own assessment of their patients, especially in straightforward cases, and avoids the potential barrier of waiting on a MHP referral. However, all specialists in Moncton currently follow the WPATH standards of care and expect a letter from a MHP to accompany referrals. As management continues to evolve and more primary care providers become component trans healthcare providers, these prerequisites will likely change, and referrals from a competent primary care provider would likely be accepted even at this point in time. Besides a formal diagnosis of gender dysphoria, other indications for a mental health referral include: uncertainty regarding the diagnosis of gender dysphoria, presence of additional complicating psychiatric diagnoses, or if the patient would benefit from psychosocial support or counselling. Patients may also appreciate information on local support groups.
- Non-gender issues: It is important to make note of any red flags that came up during the conversation that may need to be readdressed if there is no time left during the appointment (e.g. smoking cessation, bullying, overdue pap, STI screening, etc.). The transgender population is less likely to have received appropriate preventative care in the past so it is important that this is not forgotten about. See Screening and Preventative Care for more detail. A patient’s gender identity is only a small piece of their overall health and wellbeing and routine health maintenance should not be overshadowed by issues surrounding transitioning. Studies show that transgender patients appreciate when they can have their non-gender needs addressed in an environment that is not focused on their gender.
- Hormones: If a patient is interested in starting hormones, you can either refer to a local specialist (remember a formal diagnosis is needed first) or you can see Medical Management for more information. Briefly though, during the next several appointments if you choose to manage this patient independently you will have to: (1) have the patient officially diagnosed with gender dysphoria either by yourself or another qualified mental health professional; (2) determine any contraindications or patient-specific risks to cross-hormone therapy and manage as needed; (3) order and review baseline bloodwork; (4) discuss hormone options as well as the risks and benefits with the patient; (5) discuss realistic expectations of the physical changes brought on by cross-sex hormones; (6) have the patient review and sign a contract (optional, but recommended) or obtain and document informed consent.
- Surgery: If a patient is interested in pursuing surgery see Surgical Management for more information. Different types of surgeries require certain numbers of referral letters, and some surgeries must be preceded by cross-sex hormone therapy. Also, not all procedures are offered in the New Brunswick area, and patients have to travel to Montreal for genital surgery.
Remember: Treatment should be individualized
The management if each transgender patient is guided by the individual and what they feel they need to achieve gender affirmation. Not all patients will want cross-sex hormones or surgery. You may have patients that feel comfortable with only non-medical management (e.g., dressing a certain way, hair removal). In all patients it is particularly important to monitor their psychosocial health. At some point in the course of their care, most patients will benefit from seeing a mental health professional who is knowledgable in the management of gender dysphoria as this population is more likely to experience mental illness, self harm, discrimination, and abuse.
- Diagnosis
- Screening and Preventative Care
- Mental Health
- Non-Medical Management
- Medical Management
- Surgical Management
 |